Not all mobility loss begins with a dramatic fall or apparent injury. In many cases, it starts with something easy to ignore: a mild tingling in the foot, occasional leg weakness, or a strange numbness in the arm. These early signals often point to an underlying issue that’s both invisible and underestimated: nerve compression.
Over time, compressed nerves can quietly reshape how you move, balance, and function. And if left unaddressed, this disruption can evolve from a minor nuisance to a significant obstacle, impacting your gait, muscle strength, coordination, and independence.
What Is Nerve Compression and Why Does It Matter?
Nerve compression happens when a nerve is squeezed or irritated by surrounding tissues. This can be due to:
- Herniated discs or spinal degeneration
- Bone spurs from arthritis
- Tight or inflamed muscles
- Poor posture or prolonged static positions
- Repetitive movements (e.g., typing, lifting)
- Scar tissue from past injuries or surgery
Poor posture is a common yet often underestimated cause of nerve compression, particularly in the neck and lower back. Learn how bad posture contributes to chronic back pain and long-term mobility issues.
When pressure is applied to a nerve, it disrupts the signals flowing between your brain and body. This results in symptoms like pain, tingling, numbness, and weakness. However, beyond discomfort, these disruptions gradually impair how your muscles contract, your balance, and your ability to move confidently through daily life.
Early Symptoms That Often Go Unnoticed
Because nerve compression often develops gradually, its symptoms can be easily dismissed. But even mild nerve disruptions can have compounding effects on your mobility. Keep an eye out for:
- Intermittent tingling or numbness in limbs
- Sharp, shooting pain (often radiating along the nerve path)
- Weakness in one arm or leg
- A “heavy” feeling in the limbs
- Muscle fatigue after minimal activity
- Frequent tripping or imbalance while walking
These early signs may seem minor, but they can mark the beginning of a long-term functional decline.
How Nerve Compression Gradually Undermines Mobility
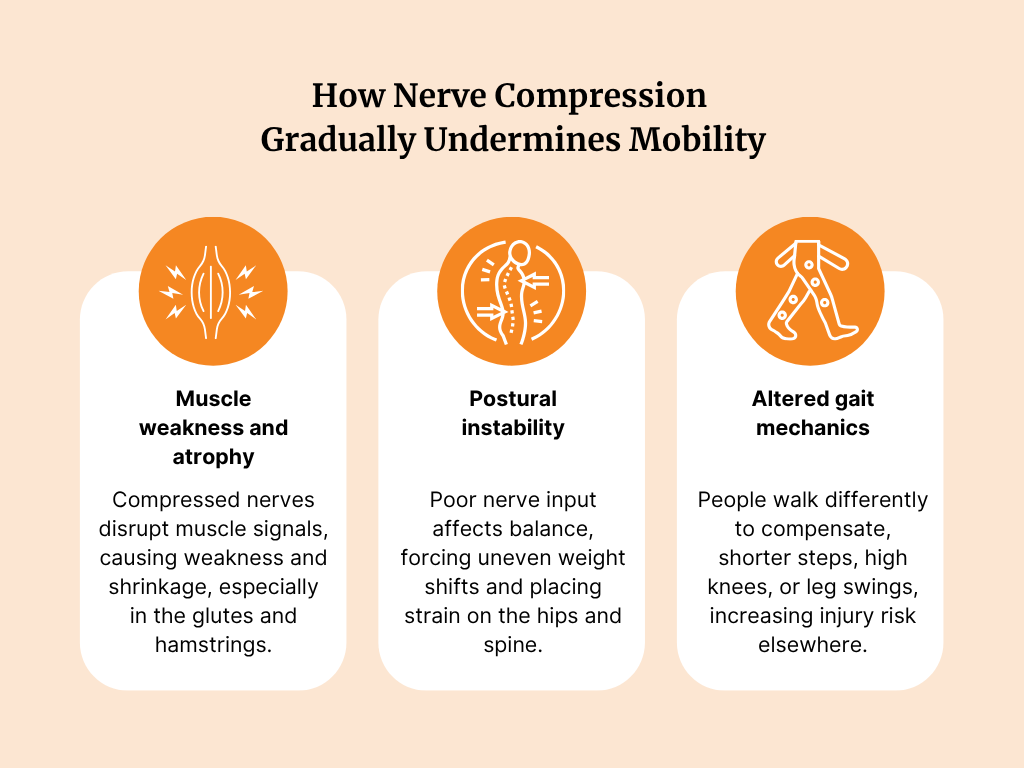
The nervous system controls every aspect of movement, from subtle postural adjustments to large-scale actions such as walking or lifting. When a nerve is compressed, these systems begin to falter.
Here’s what that breakdown can look like:
1. Muscle Weakness and Atrophy
Muscles rely on nerve signals to contract effectively. When nerves are compressed, signals may weaken or stop altogether, leading to muscle underuse and, eventually, atrophy. For example, compression of the sciatic nerve can weaken the gluteal and hamstring muscles, making activities such as stair climbing or rising from a chair increasingly challenging.
2. Postural Instability
Loss of coordination and proprioception (your sense of body position) can affect balance. People may begin to shift weight unevenly or walk with a broader stance to feel more stable, often placing excess strain on the hips and spine.
3. Altered Gait Mechanics
To compensate for nerve-related weakness or foot drop, many people adjust their walking style, taking shorter steps, lifting their knees higher, or swinging the affected leg outward. These adaptations may relieve symptoms in the short term, but often lead to overuse injuries elsewhere in the body.
Common Compression Sites That Affect Movement
Different nerves control different parts of the body, and compression in each location can lead to unique mobility challenges:
- Sciatic nerve (lower back): Radiating pain, leg weakness, difficulty standing or walking
- Peroneal nerve (outer knee): Foot drop, toe drag, gait asymmetry
- Cervical nerves (neck): Reduced grip strength, shoulder stiffness, poor upper body coordination
- Median nerve (wrist): Numbness in fingers, weak grip, impaired dexterity
Even minor compression in these areas can disrupt your body's balance and coordination over time.
When the Body Compensates and Why That’s a Problem
The human body is adaptive. When one area becomes weak or unresponsive, others jump in to compensate. But this strategy doesn’t always work in your favour.
For instance:
- A weakened ankle may lead to overuse of the hips and knees
- Poor grip strength may shift strain to the shoulders and neck
- Altered posture from back pain may compress other nerves further
These domino effects are subtle at first but can spiral into more widespread musculoskeletal dysfunction. This is why addressing the root, not just the symptom, is crucial.
Real-World Signs of Reduced Mobility Due to Nerve Compression
The effects of nerve compression often show up in simple, everyday activities:
- Difficulty maintaining balance on uneven ground
- Climbing stairs with one leg leading every time
- Hesitation when stepping off curbs
- Needing arm support to stand from a low seat
- Losing grip on small objects like pens or utensils
- Feeling fatigued after short walks or minor chores
These aren’t just signs of ageing. They may signal that your nervous system isn’t communicating effectively with your muscles.
The Cost of Waiting Too Long
Delaying treatment for nerve compression can result in:
- Permanent nerve damage
- Muscle wasting that cannot be reversed
- Increased fall risk due to poor balance and coordination
- Widespread compensatory injuries
- Chronic pain and reduced independence
As the condition worsens, even routine interventions may be less effective. Early detection and treatment offer the best chance to preserve function and mobility.
What You Can Do: Strategies That Support Nerve Health and Mobility
Recovery depends on the severity and duration of the compression, but many cases improve significantly with conservative care.
If you are looking to prevent future compression, spinal mobility exercises can be just as crucial as building core strength for maintaining nerve space and healthy movement.
Here’s what a proactive plan may include:
1. Physiotherapy
Targeted exercises help relieve pressure, restore mobility, and rebuild strength in affected muscles.
2. Posture and Ergonomics
Correcting daily habits, especially for those in desk-based or repetitive roles, can help prevent worsening compression.
3. Manual Therapy and Nerve Gliding
Hands-on techniques and movement protocols may release adhesions and restore nerve mobility.
4. Footwear and Supportive Devices
Custom orthotics, braces, or mobility aids can support proper gait mechanics and offload pressure from affected nerves.
5. Lifestyle Modifications
Incorporating low-impact activities, improving sleep, and reducing inflammation through a balanced diet can all support nerve repair and overall musculoskeletal function.
.png)
In severe or chronic cases, further investigations and interventions, such as injections or surgery, may be required; however, most people benefit significantly from early, non-invasive care.
Final Takeaway
Nerve compression doesn’t always show. It whispers. However, those whispers, tingling, weakness, and subtle imbalances can grow louder over time. If left unchecked, they can change how you walk, move, and live.
Just like psychological needs, physical mobility sits at the foundation of long-term well-being. Our interpretation of Maslow’s hierarchy for musculoskeletal health highlights why restoring nerve function is crucial to regaining independence.
By recognising early signs and taking action before symptoms escalate, you can safeguard your long-term mobility and quality of life. You don’t need to wait for a crisis. You just need to listen and respond.
References
- Cleveland Clinic: Nerve Compression Syndrome
- NCBI: Peripheral Neuropathy Overview
- Healthline: Nerve Compression Syndrome
- Elite Family Chiropractic: Living With Neuropathy
- Cleveland Clinic: Peripheral Neuropathy
- Aspetar Journal: Common Peroneal Nerve Compression in Athletes
- Nuffield Clinic: Nerve Damage and Mobility
This article is reviewed by Dr. Anurag Gupta, a gold medalist in MPT-Sports Physiotherapy, has worked with elite international and national athletes across football, tennis, and badminton. His clientele includes Srikanth Kidambi (#1 Men’s Badminton Player, Arjuna Awardee, Padma Shri) and Hendra Setiawan (Olympic Gold Medalist, 4x World #1 in Men’s Badminton).
Beyond athletes, Dr. Gupta is the preferred physiotherapist for top founders, including Vivek Gupta (Licious), Rishabh Telang (Cult.fit), and Arjun Chaudhary (former MFine), helping them recover from musculoskeletal issues efficiently.










