Knee Osteoarthritis: Molecular Biomarkers for Early Detection
Introduction
Knee osteoarthritis (OA) is fast becoming one of the most common and disabling joint conditions in India. Approximately 45% of adults over the age of 50 in India show clinical or radiographic signs of knee osteoarthritis.
As life expectancy increases and sedentary lifestyles become more widespread, particularly in urban areas, the burden of joint pain is growing rapidly.
Women over the age of 50, individuals with obesity, and those with a history of joint injuries are particularly at risk.
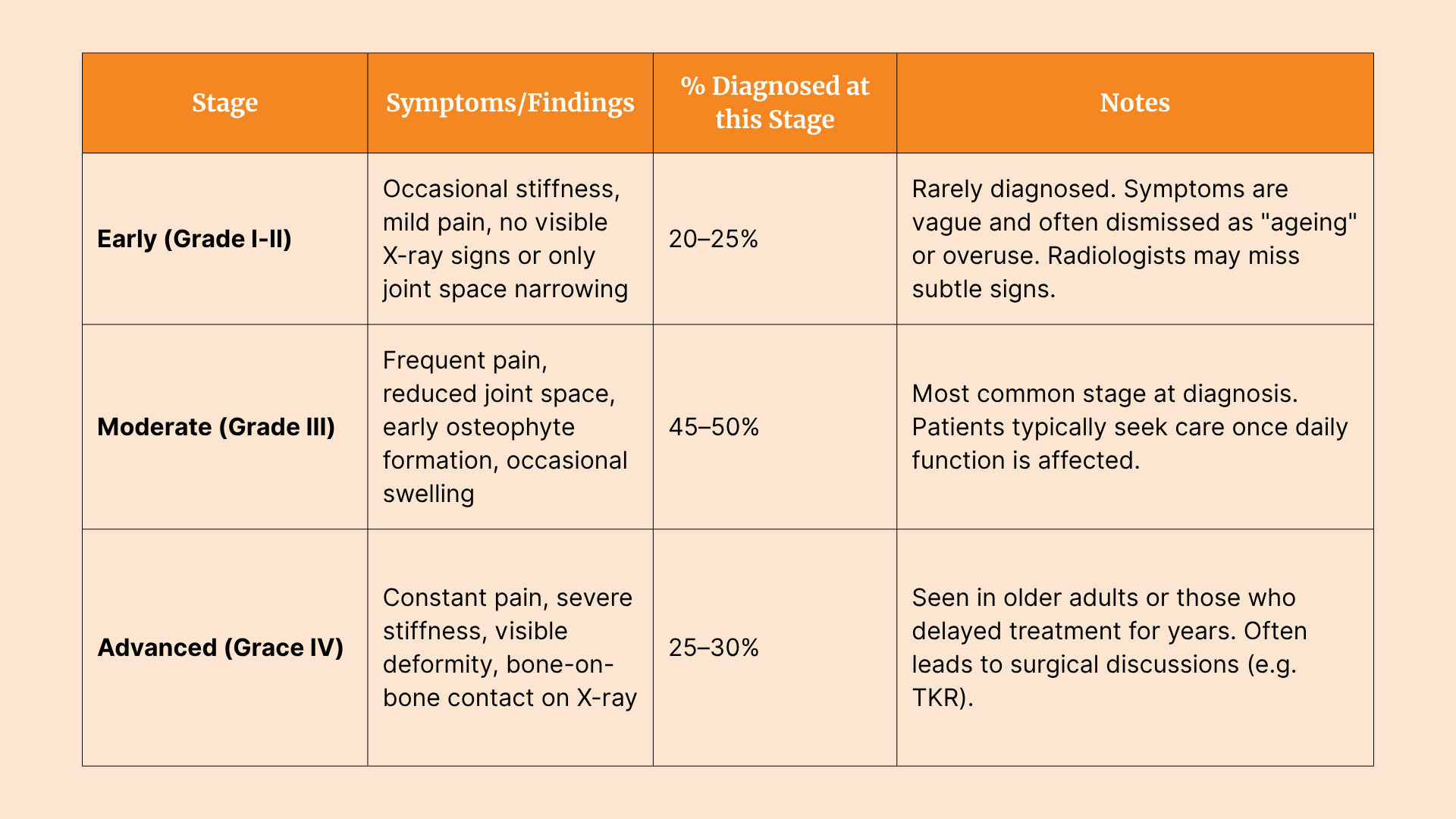
A recent study found that Knee OA diagnosis in India happens very late. Despite this, OA is still frequently diagnosed late, when damage to the joint is already advanced.
So, what is the problem with traditional diagnostic tools?
Commonly used and time-tested methods, such as X-rays or MRI scans, often detect the disease only after structural changes have occurred in the Knee joint, leaving fewer options for effective early intervention.
Recent developments in medical science, however, offer new hope. Molecular Biomarkers offer a hope for early detection and intervention.
Molecular biomarkers are biological molecules found in blood, urine or synovial fluid. These can signal the onset of joint damage or inflammation well before it is visible on imaging. Such biomarkers could help identify OA in its earliest stages, even before pain becomes chronic or cartilage loss becomes irreversible.
This raises a compelling question:
Could a simple blood, urine or joint fluid test predict your risk of knee osteoarthritis years before symptoms become severe? The Answer is YES.
With this, India could shift from a late-stage, pain-management approach to a much-needed model of early detection and joint preservation.
The Indian Context: Why Early Diagnosis Matters More Here
In India, the burden of knee osteoarthritis is rising rapidly, particularly among women over the age of 50 and individuals in urban areas who lead sedentary lifestyles.
This demographic shift, combined with dietary inadequacies and growing obesity rates, is contributing to the earlier onset and faster progression of joint degeneration. Despite this, the healthcare system remains largely reactive when it comes to musculoskeletal care.
India has covered a massive ground in terms of healthcare access. X-rays are universally accessible in most areas today, and advanced imaging, i.e. MRI, is rapidly becoming more affordable and available in secondary healthcare settings.
What are the problems?
- Indian cultural tendency to dismiss early joint pain as a natural part of ageing. Individuals delay seeking medical advice until the pain becomes disabling or starts interfering with daily activities such as climbing stairs, squatting, or walking long distances. This delay has serious consequences. By the time OA is diagnosed, many patients are already in the moderate to advanced stages of the disease, when cartilage damage is extensive
- Imaging typically detects OA only once structural changes have already occurred.
- The financial cost of Knee OA management is high. Total knee replacement (TKR), the most common surgical response to advanced OA, typically costs between ₹3 and ₹7 lakh in private hospitals. This represents a significant financial burden for most Indian families, especially when the disease is detected late and no longer manageable through conservative methods.
This is where molecular biomarkers could make a difference. By enabling early-stage detection, they allow timely lifestyle changes, physiotherapy, and joint-preserving care before the damage becomes irreversible. This can significantly reduce both clinical complications and long-term costs for patients in India.
What Are Molecular Biomarkers and Which Ones Matter for Knee OA?
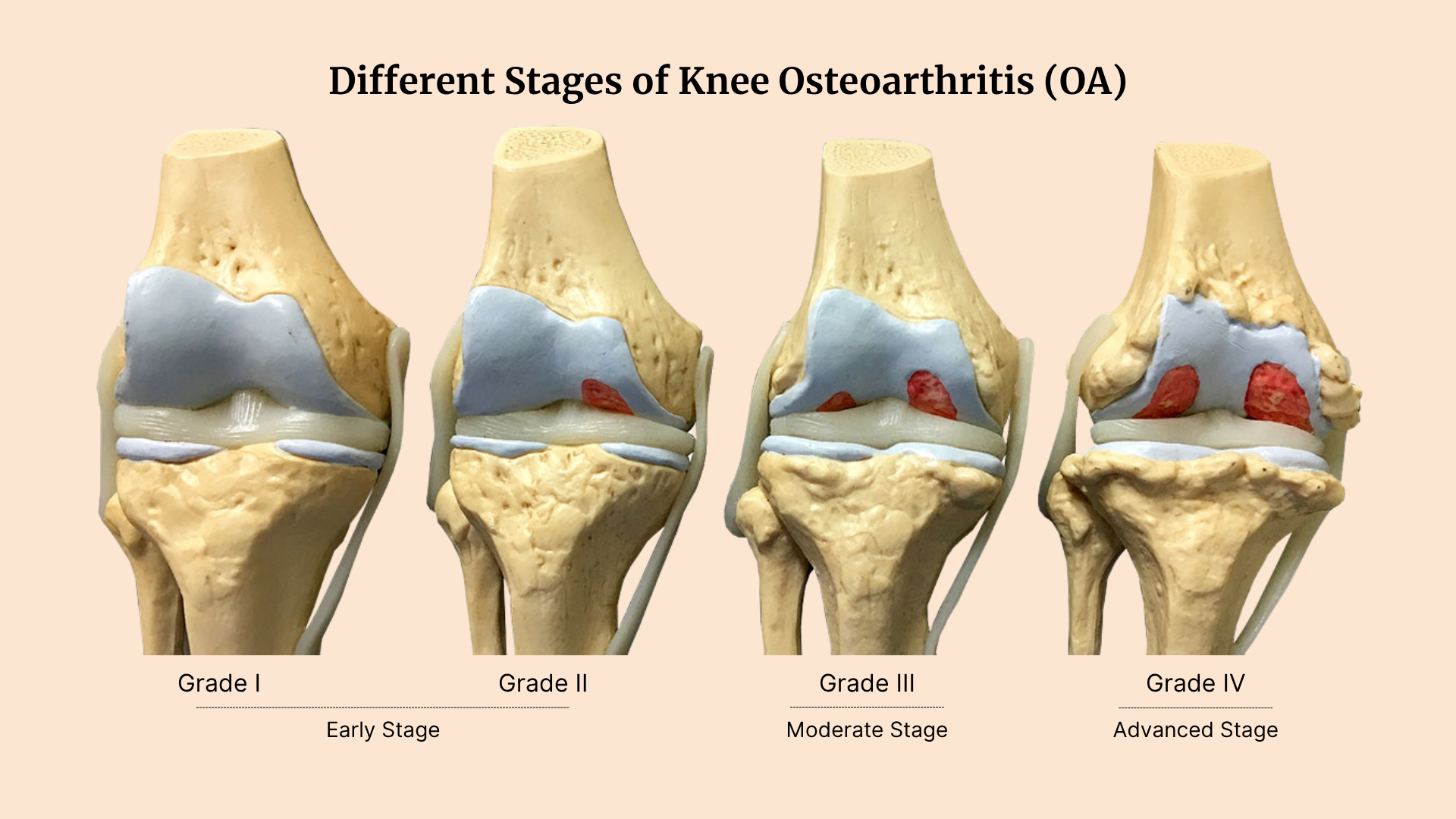
Molecular biomarkers are biological molecules such as proteins, enzymes or genetic fragments that provide measurable signs of physiological processes occurring within the body. For knee osteoarthritis, these biomarkers can signal early cartilage damage, joint inflammation or changes in bone metabolism well before such issues appear on X-rays or MRI scans. They are typically detected through non-invasive samples like blood, urine or synovial fluid. Here are some molecular biomarkers and what they measure.
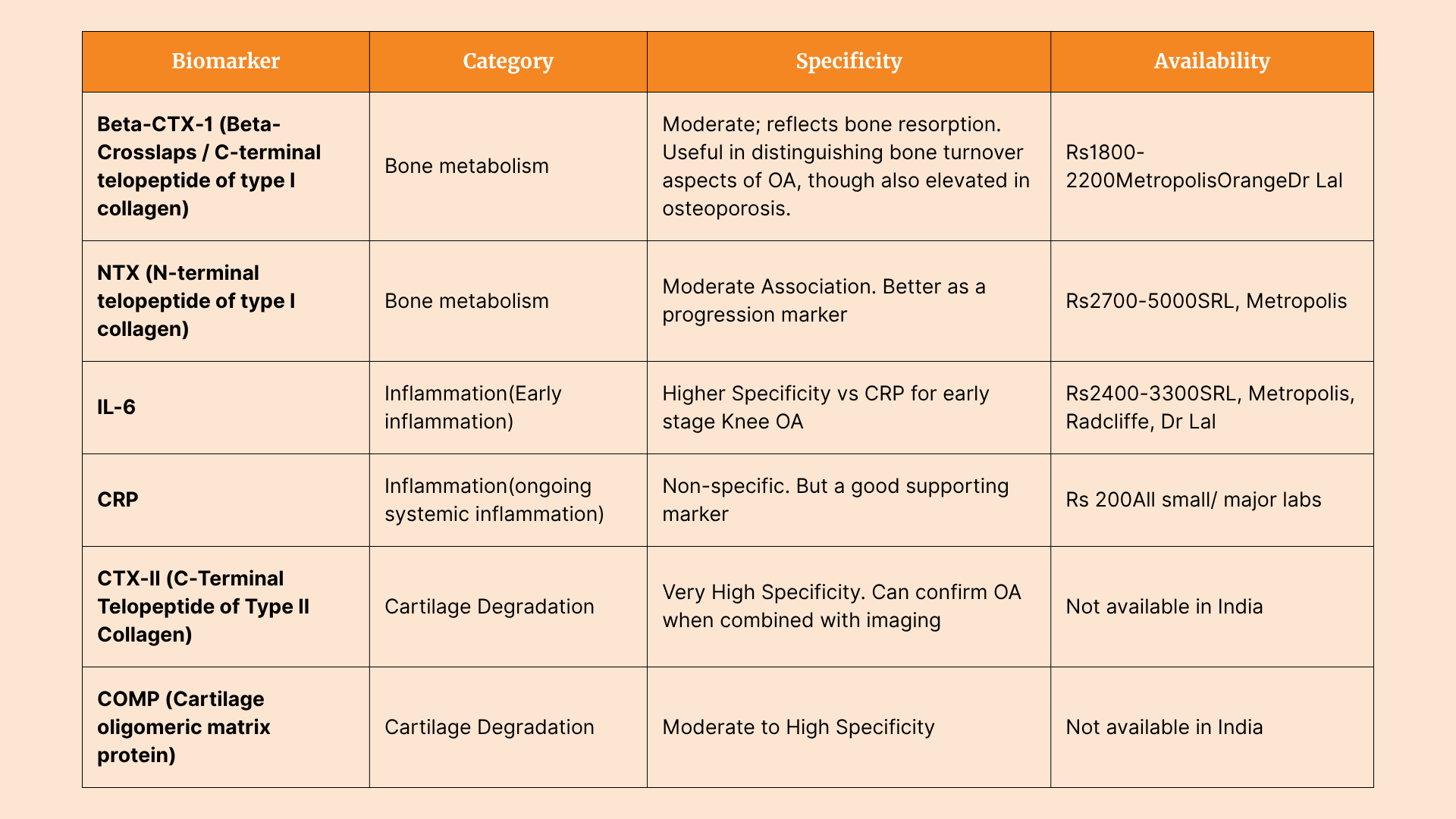
The most clinically relevant biomarkers fall into three categories:
- Inflammatory markers, such as interleukin‑6 (IL‑6) and C‑reactive protein (CRP), provide evidence of systemic or local inflammation around the joint
- Cartilage degradation markers, including CTX‑II (C‑terminal telopeptide of type II collagen), COMP (cartilage oligomeric matrix protein) and MMPs (matrix metalloproteinases), directly reflect cartilage breakdown
- Bone metabolism markers, such as NTX (N‑telopeptide of type I collagen) and osteocalcin, indicate changes in subchondral bone turnover.
Relevance to Indian Patients: The ₹8,000 Test You Should Gift Your Parent or Yourself
Knee OA in India often develops under a unique mix of mechanical and inflammatory stress. With rising rates of obesity and metabolic syndrome, many Indians carry a higher inflammatory load, which accelerates joint damage.
Common dietary patterns, low in calcium and protein but high in carbohydrates, further weaken cartilage.
As a result, biomarkers like Beta CTX, NTX become especially relevant in identifying early, hidden joint damage in Indian patients.
For anyone with a family history of joint issues or early symptoms, investing in a ₹8,000 biomarker panel could be a powerful step toward prevention and early care.
How Early Detection Could Change OA Diagnosis and Management - From Reactive to Proactive Care
Early identification of individuals at risk for knee OA through molecular biomarkers offers a critical opportunity to shift from reactive to proactive care. Detecting OA in its early stages allows for timely lifestyle interventions such as weight management and strength training, which can help reduce joint stress and delay progression. It also creates space for preventive strategies, including the use of supportive orthotic devices or targeted nutritional supplementation to maintain joint health. Biomarker-based screening could be integrated into health programmes, particularly for high-risk populations like postmenopausal women and individuals with diabetes.
Collectively, these measures have the potential to transform musculoskeletal care in India by focusing on prevention and long-term joint preservation, rather than waiting until surgery becomes the only option.
But There Are Challenges
Despite the promise of molecular biomarkers in transforming knee osteoarthritis care, several challenges remain, particularly in the Indian context.
First, the cost and limited availability of specialised biomarker tests such as CTX-II, or COMP restrict their use to research settings or tertiary hospitals.
These tests are not routinely offered in commercial labs, making them inaccessible to most patients.
Second, there is a lack of standardisation and validation for the Indian population, which differs genetically and epidemiologically from Western cohorts where most biomarker studies have been conducted. This limits the clinical applicability of global reference values. Another major hurdle is clinician awareness. Many orthopaedic doctors continue to rely primarily on X-rays, which detect OA only at advanced stages.
Finally, for biomarkers to be widely adopted, they must be supported by regulatory frameworks and covered under insurance schemes, neither of which is in place today.
Bridging these gaps will be essential for biomarkers to play a meaningful role in routine OA diagnosis and management across India.
What Needs to Happen Next
India needs local research cohorts to validate OA biomarkers in its population, led by institutions like AIIMS and supported by ICMR. Public-private partnerships should focus on making these tests affordable and accessible. At the same time, clinicians must be trained to recognise the value of biomarkers in early diagnosis, moving beyond the current reliance on late-stage imaging.
Conclusion
Molecular biomarkers have the potential to transform the way knee osteoarthritis is diagnosed in India, where most patients currently present only after significant joint damage has occurred. For this promise to be realised, India must invest in research, make testing more affordable, and integrate biomarkers into routine clinical practice. The path to preventing OA, rather than simply managing its late effects, begins with detecting it early.
References
A 2020 study published in the International Journal of Community Medicine and Public Health found that 47.3% of people aged 50 and above had symptomatic knee OA in semi-urban South India.
Can urinary CTX-II be a biomarker for knee osteoarthritis? | Arthroplasty | Full Text
This article is reviewed by Dr. Anurag Gupta, a gold medalist in MPT-Sports Physiotherapy, has worked with elite international and national athletes across football, tennis, and badminton. His clientele includes Srikanth Kidambi (#1 Men’s Badminton Player, Arjuna Awardee, Padma Shri) and Hendra Setiawan (Olympic Gold Medalist, 4x World #1 in Men’s Badminton).
Beyond athletes, Dr. Gupta is the preferred physiotherapist for top founders, including Vivek Gupta (Licious), Rishabh Telang (Cult.fit), and Arjun Chaudhary (former MFine), helping them recover from musculoskeletal issues efficiently.










