Inflammation is the body's natural defence mechanism against injury and infection. When controlled and acute, it is essential for healing. However, when inflammation becomes chronic, it can turn against the body, leading to widespread tissue damage, including within the joints. Joint degeneration, often associated with osteoarthritis and rheumatoid arthritis, is deeply intertwined with the body's inflammatory processes. Understanding how chronic inflammation fuels joint degeneration is vital for prevention, early intervention, and effective management.
What Is Chronic Inflammation?
Acute inflammation is a short-term response characterised by redness, swelling, heat, and pain, aimed at removing harmful stimuli and initiating repair. Chronic inflammation, in contrast, is a prolonged, low-grade inflammatory response that persists over months or years, often silently damaging tissues without obvious signs until significant deterioration has occurred.
Common causes of chronic inflammation include autoimmune disorders, persistent infections, exposure to irritants, and lifestyle factors such as poor diet, stress, and physical inactivity. Key markers of chronic inflammation include elevated levels of C-reactive protein (CRP), interleukin-6 (IL-6), and tumour necrosis factor-alpha (TNF-α).
How Inflammation Damages Joints
1. Synovial Inflammation
Joints are surrounded by the synovial membrane, a soft tissue that produces synovial fluid for lubrication. Chronic inflammation leads to synovitis, where this membrane thickens and produces excess fluid rich in inflammatory mediators. This triggers pain, swelling, and stiffness, while enzymes within the fluid begin degrading cartilage.
2. Cartilage Breakdown
Cartilage is a rigid yet flexible tissue that cushions joints. Inflammatory cytokines such as IL-1β and TNF-α stimulate the production of enzymes like matrix metalloproteinases (MMPs), which degrade cartilage matrix components, including collagen and proteoglycans. Without healthy cartilage, bones rub against each other, leading to joint damage and pain.
3. Bone Erosion
In conditions like rheumatoid arthritis, chronic inflammation activates osteoclasts, the cells responsible for bone resorption. This leads to bone erosion around joints, causing deformity, instability, and loss of function.
4. Ligament and Tendon Damage
Inflammatory processes can also weaken ligaments and tendons that support the joints. Over time, these structures lose their tensile strength, contributing to joint instability and a higher risk of injury.
Common Conditions Linking Chronic Inflammation and Joint Degeneration
- Osteoarthritis (OA): Traditionally seen as a "wear-and-tear" disease, recent evidence shows low-grade inflammation plays a significant role in OA progression.
- Rheumatoid Arthritis (RA): An autoimmune disease where chronic inflammation primarily targets synovial joints, leading to severe joint damage and systemic symptoms.
- Psoriatic Arthritis: Inflammatory arthritis is associated with psoriasis and causes joint pain, stiffness, and swelling.
- Ankylosing Spondylitis: Chronic inflammation of the spine and large joints, leading to fusion and loss of mobility.
Mechanisms Behind Chronic Inflammation and Joint Damage
Immune System Dysregulation
Chronic inflammation often stems from a misdirected immune system that mistakenly attacks healthy tissues. In RA, for example, the immune system targets the synovium, resulting in aggressive inflammation that damages joints.
Oxidative Stress
Persistent inflammation generates reactive oxygen species (ROS) that damage DNA, proteins, and cell membranes. This oxidative stress further fuels joint tissue degradation.
Imbalance of Pro and Anti-Inflammatory Factors
Healthy inflammation resolves once the threat is neutralised. However, in chronic inflammation, there is an imbalance between pro-inflammatory cytokines and anti-inflammatory molecules, leading to unregulated tissue destruction.
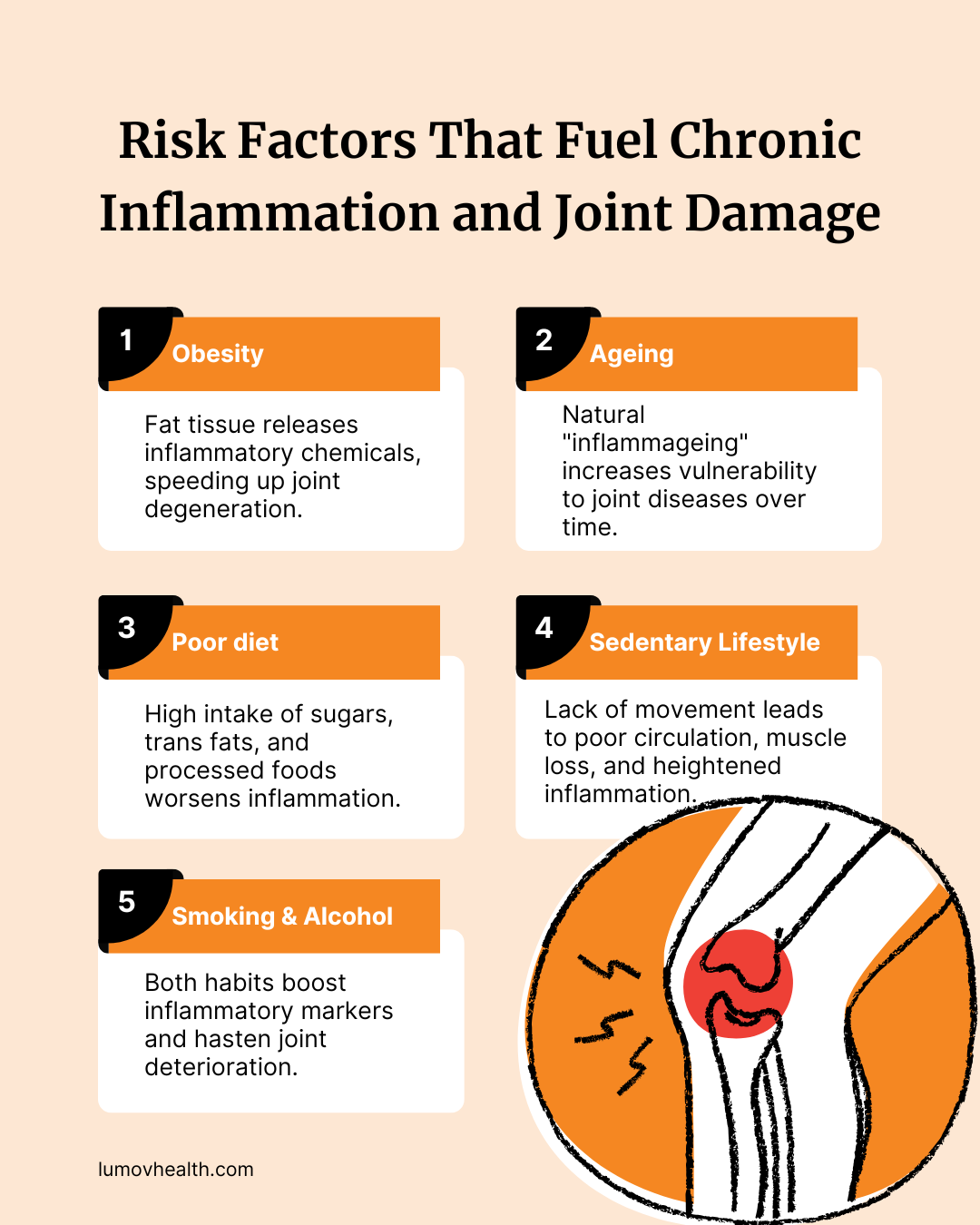
Risk Factors Amplifying Chronic Inflammation and Joint Degeneration
Obesity
Adipose (fat) tissue is not inert; it secretes inflammatory cytokines, particularly IL-6 and TNF-α. Obesity thus creates a state of systemic low-grade inflammation, accelerating joint wear and tear.
Ageing
Ageing is naturally associated with increased inflammatory activity, termed “inflammageing.” This predisposes older adults to degenerative joint diseases.
Diet
Diets high in refined sugars, trans fats, and processed foods promote systemic inflammation. Anti-inflammatory diets rich in fruits, vegetables, omega-3 fatty acids, and whole grains may help counteract these effects.
Sedentary Lifestyle
Physical inactivity contributes to poor circulation, muscle atrophy, and fat accumulation, all of which exacerbate inflammatory responses in the body.
Smoking and Alcohol Consumption
Both smoking and excessive alcohol intake elevate inflammatory markers and are linked to accelerated joint degeneration.
Early Signs of Chronic Inflammation Affecting Joints
- Persistent joint pain or stiffness
- Swelling and warmth around joints
- Fatigue and malaise
- Morning stiffness lasting more than 30 minutes
- Reduced range of motion
Recognising these signs early and seeking medical attention is critical to prevent irreversible joint damage.
Managing Chronic Inflammation to Protect Joint Health
1. Anti-Inflammatory Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are commonly prescribed to reduce inflammation and relieve pain. Disease-modifying antirheumatic drugs (DMARDs) are vital for autoimmune conditions like RA.
2. Lifestyle Changes
- Exercise Regularly: Low-impact activities like swimming, cycling, and yoga help maintain joint flexibility and muscle strength.
- Adopt an Anti-Inflammatory Diet: Focus on foods rich in antioxidants and omega-3 fatty acids, such as salmon, walnuts, and leafy greens.
- Maintain a Healthy Weight: Reducing excess body weight alleviates pressure on weight-bearing joints.
- Quit Smoking and Limit Alcohol: Both habits worsen systemic inflammation.
3. Supplements and Alternative Therapies
Omega-3 supplements, curcumin (found in turmeric), and green tea extract have anti-inflammatory properties. Physiotherapy and occupational therapy can also help in joint preservation and functional rehabilitation.
4. Emerging Therapies
Research into biologics—targeted therapies that inhibit specific inflammatory mediators—shows promising results in halting joint degeneration. Regenerative therapies, such as platelet-rich plasma (PRP) and stem cell injections, are also under investigation.
Preventing Chronic Inflammation: A Proactive Approach
While genetics and age are unavoidable factors, many contributors to chronic inflammation are within our control. Simple proactive steps include:
- Prioritising sleep hygiene
- Managing stress through mindfulness and relaxation techniques
- Staying active
- Consuming a nutrient-dense, anti-inflammatory diet
An integrated approach combining medical management with lifestyle interventions offers the best chance to slow or prevent joint degeneration.
Conclusion: Nipping the Flame in the Bud
Chronic inflammation is a symptom and a driving force behind joint degeneration. Its insidious nature means damage can accumulate silently for years before noticeable symptoms appear. However, with growing understanding of its mechanisms and risk factors, there is immense potential for prevention and intervention.
Recognising the signs early, adopting anti-inflammatory strategies, and working closely with healthcare providers can help preserve joint health and quality of life. In the battle against joint degeneration, tackling chronic inflammation head-on is beneficial and essential.
References
- [1] Chronic Inflammation - National Center for Biotechnology Information (NCBI) Bookshelf: https://www.ncbi.nlm.nih.gov/books/NBK493173/
- [2] Cleveland Clinic: Inflammation Overview: https://my.clevelandclinic.org/health/symptoms/21660-inflammation
- [3] The role of inflammation in the pathogenesis of osteoarthritis - PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC3327731/
- [4] ScienceDirect: Inflammation and osteoarthritis: https://www.sciencedirect.com/science/article/pii/S2352320420300651
- [5] Harvard Health Publishing: How acute inflammation turns chronic: https://www.health.harvard.edu/healthbeat/how-acute-inflammation-turns-chronic
- [6] ScienceDirect: Cytokines and their role in inflammation and arthritis: https://www.sciencedirect.com/science/article/pii/S1063458415011735
- [7] WebMD: Chronic Inflammation and Arthritis: https://www.webmd.com/rheumatoid-arthritis/features/chronic-inflammation-link
- [8] WebMD: Unexpected Signs of Chronic Inflammation: https://www.webmd.com/arthritis/ss/slideshow-signs-chronic-inflammation-unexpected










