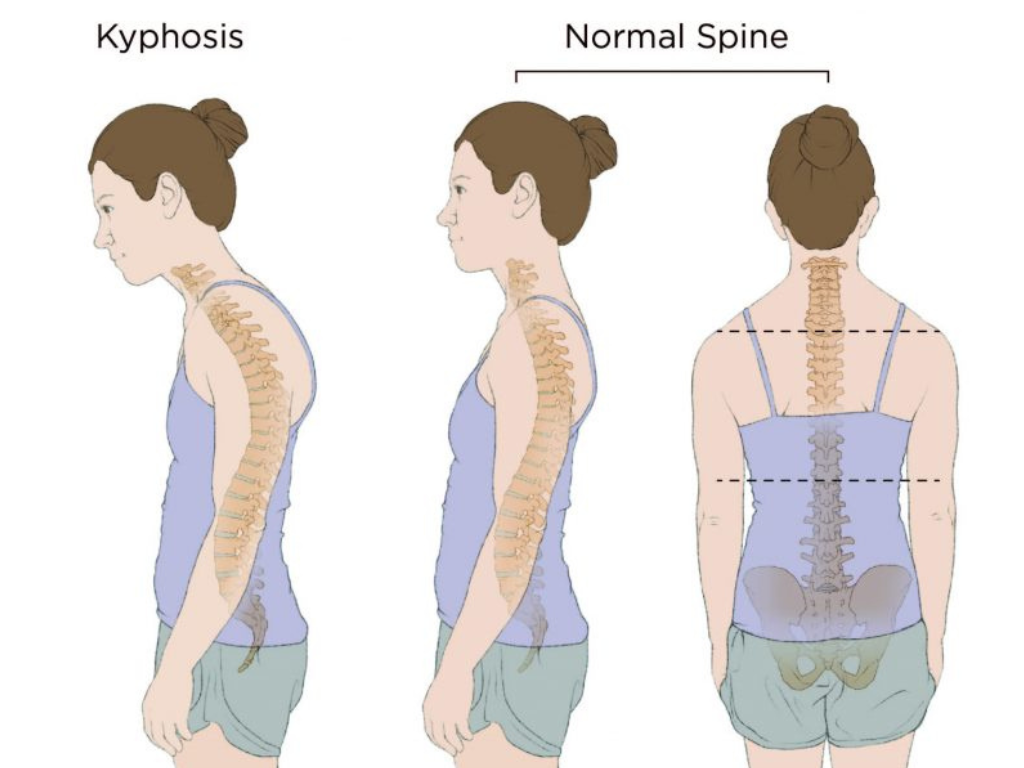
A subtle curve in the upper back may seem harmless, but it can also lead to bad posture. However, when that curve deepens and starts affecting your movement, breathing, or confidence, it may be a sign of something more serious: kyphosis. For many women over 40, this condition develops silently and gradually, often dismissed as an inevitable part of ageing. But understanding the early symptoms of kyphosis and seeking timely care can make a significant difference.
This guide breaks down what kyphosis looks like in women over 40, how to identify its signs, and what to do next.
Why Kyphosis Symptoms Matter More in Menopause
Kyphosis can occur at any age, but after 40, the body goes through structural and hormonal shifts that increase vulnerability. For women, the drop in estrogen levels around menopause accelerates bone density loss (osteopenia and osteoporosis). This makes the spinal vertebrae more fragile and prone to collapse. Simultaneously, age-related muscle loss (sarcopenia) reduces the ability to support upright posture.
What does this mean in everyday life? A gradual stooping of the shoulders, unexplained back pain, or reduced flexibility are not just cosmetic or lifestyle issues. They could be signs of a progressive spinal condition. Ignoring early symptoms of kyphosis could lead to pain, functional loss, and even respiratory or neurological problems later on.
Where Kyphosis Fits in the MSK Health Equation
Postural Kyphosis
Often seen in younger people, poor posture in women over 40 can be exacerbated by long hours at desks, weak core/back muscles, and a lack of movement, which can accelerate structural changes already occurring due to ageing.
.png)
Osteoporotic Kyphosis
This is the most serious form in older women. As bones weaken, the vertebrae in the upper spine may compress and collapse, causing a hunched back (widow’s hump). This form is often permanent if not caught early.
Degenerative Kyphosis
With age, spinal discs and ligaments wear out. This can lead to curvature, pain, and nerve impingement. Degenerative kyphosis progresses slowly but can significantly impact mobility and quality of life.
7 Early Symptoms of Kyphosis in Women Over 40
Spotting kyphosis early is crucial for managing it effectively. Here are key symptoms to watch for:
1. Rounded upper back (Hunched Posture)
You may notice your shoulders rounding forward or a visible curve forming at the top of your spine. Others might see your profile changing, even before you feel discomfort.
2. Back pain or stiffness
Dull, aching pain in the upper back is common, particularly after prolonged periods of standing or sitting. Stiffness may make it harder to rotate your spine or reach overhead.
3. Loss of height
Have you lost an inch or more in height over the years? Vertebral compression due to osteoporosis-related fractures can gradually shorten your spine.
4. Fatigue in the back or legs
Supporting a curved spine takes effort. Many women experience back fatigue, particularly toward the end of the day or after engaging in an activity.
5. Breathing difficulties
As the spine curves forward, the chest cavity may lose space. This can reduce lung expansion, leading to shortness of breath during routine activities.
6. Stiff hamstrings or loss of flexibility
Muscle imbalances and tightness often accompany kyphosis. Hamstrings, hip flexors, and spinal muscles can become less flexible, leading to a worsening of posture.
7. Neurological symptoms (in advanced cases)
If kyphosis progresses and compresses the spinal cord or nerves, it may lead to numbness, tingling, or weakness in the arms or legs.
Key Risk Factors for Women after Menopause
These are the major contributors to kyphosis after 40, in order of severity:
1. Osteoporosis and vertebral fractures
The most common and serious cause. Brittle bones collapse under normal weight, causing curvature.
2. Loss of muscle mass (Sarcopenia)
Weakened back muscles reduce your ability to maintain posture. Without muscular support, the spine naturally begins to bend forward.
3. Degenerative disc disease
Age-related wear and tear of the spinal discs decrease disc height and shift spinal alignment, leading to progressive curvature.
4. Changes in connective tissue
Ligaments and tendons lose elasticity with age and hormonal changes. Weakened support structures allow the spine to sag.
5. Lifestyle and postural habits
Prolonged sitting, slouched posture, heavy bags, and low physical activity contribute to and accelerate structural changes, although they are rarely the primary cause.
When Should You See a Doctor for Kyphosis?
If you experience any of the following, it is essential to consult a healthcare professional:
- A visible or increasing curve in your upper back
- Chronic back pain or stiffness
- Difficulty standing straight for long durations
- Shortness of breath or pressure in the chest
- Tingling, numbness, or weakness in the arms or legs
- Difficulty with balance, walking, or coordination
- Fever with back symptoms (this may indicate infection or inflammation)
Early intervention not only helps in diagnosing the root cause but can also slow or stop the progression of kyphosis. Your doctor may recommend imaging tests, such as X-rays, bone density scans, or MRIs, to identify structural or neurological involvement.
Common Myths and Misunderstandings about Kyphosis
Let us bust a few widespread misconceptions:
.png)
Long-term impact of ignoring symptoms
Neglecting the signs of kyphosis can lead to serious and sometimes irreversible consequences:
- Worsening spinal curvature
- Chronic, disabling back pain
- Reduced mobility and independence
- Breathing difficulty due to compressed lungs
- Neurological symptoms such as tingling or balance problems
- Psychosocial distress: depression, low self-esteem, and isolation
- Impaired digestion in extreme cases
The sooner you act, the better the chances of slowing the curve, relieving symptoms, and maintaining a high quality of life.
Frequently Asked Questions (FAQs)
1. Is Kyphosis reversible in women over 40?
Mild postural kyphosis may be improved with targeted exercises and physiotherapy. However, structural kyphosis due to bone or disc degeneration is usually permanent but can be managed.
2. Can Kyphosis go away on its own?
No. Without addressing the underlying causes, such as weak bones or muscles, it typically progresses. Early intervention is crucial for managing symptoms and slowing disease progression.
3. What type of doctor should I see for Kyphosis?
Start with a primary care doctor. You may be referred to a spine specialist, an orthopaedic surgeon, or a physiotherapist, depending on the severity of your condition.
4. How is Kyphosis diagnosed?
Through physical examination, X-rays to measure curvature angle, and bone density tests to assess osteoporosis. MRI may be required in advanced cases.
5. Can exercises really help?
Yes. Strengthening the back extensors, improving core stability, and stretching tight muscles can reduce symptoms and improve posture.
References
- Sinaki, M. (2017). Osteoporosis-related kyphosis and posture training. Mayo Clinic Proceedings.
- Katzman, W. B., Vittinghoff, E., Kado, D. M. (2016). Spine curvature and mobility in older women. Journal of the American Geriatrics Society.
- Glassman, S. D. et al. (2005). Impact of spinal deformity on quality of life. Spine Journal.
- National Osteoporosis Foundation. (2024). Understanding Kyphosis.
- WHO (2023). Musculoskeletal conditions and aging.

.png)








