Spinal surgery offers hope to millions seeking relief from debilitating back conditions. However, for a small percentage of patients, what should be a journey toward recovery becomes a medical emergency. Post-operative cauda equina syndrome (CES) represents one of the most serious complications following lumbar spine surgery, occurring in approximately 0.08% to 2.8% of procedures. This rare but potentially devastating condition demands immediate recognition and swift intervention to prevent permanent neurological damage.
Understanding Post-Surgical Cauda Equina Syndrome
What Is Post-Operative CES?
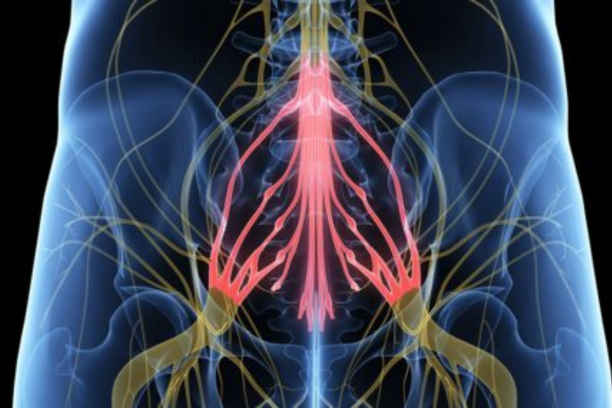
Post-operative cauda equina syndrome differs from the more commonly known CES that develops naturally from disc herniation or spinal stenosis. This condition emerges after spinal surgery, affecting the bundle of nerves at the base of the spinal cord known as the cauda equina—Latin for "horse's tail" due to its distinctive appearance.
The incidence varies significantly depending on the type of procedure. Simple discectomy carries the lowest risk at approximately 0.08%, whilst complex spinal stenosis decompressions can see rates as high as 2.8%. These statistics underscore the importance of recognising early warning signs.
Key Risk Factors for Development
Several factors increase the likelihood of developing post-operative CES:
- Advanced age (particularly patients over 65 years)
- Female gender (especially regarding long-term bladder dysfunction)
- Complex surgical procedures involving multiple vertebral levels
- Prolonged operations lasting longer than 210 minutes
- Intraoperative complications such as dural tears or significant blood loss
- Pre-existing conditions, including severe spinal stenosis or diabetes mellitus
Recognising the Warning Signs: Core Symptoms
Bladder and Urinary Dysfunction
Bladder problems represent the most common and often earliest manifestation of post-operative CES. These symptoms typically develop within the first few days after surgery.
Urinary retention stands as the hallmark symptom, affecting up to 66% of patients who develop post-operative CES. Patients find themselves unable to empty their bladder, often requiring catheter insertion after routine post-surgical catheter removal.
Overflow incontinence frequently accompanies retention, where small amounts of urine leak continuously due to an overfilled bladder. This differs from typical incontinence as patients retain some awareness but cannot control voiding effectively.
Altered bladder sensation manifests as:
- Decreased awareness of bladder filling
- Inability to sense when the bladder is full
- Complete absence of the urge to urinate
- Persistent feeling of incomplete emptying
Bowel and Defecatory Problems
Bowel dysfunction often develops alongside urinary symptoms, though it may be less immediately apparent. The impact on quality of life can be profound and long-lasting.
Faecal incontinence ranges from occasional minor leakage to complete loss of bowel control, affecting approximately 10-20% of post-operative CES patients.
Constipation and retention present as an inability to have regular bowel movements, often accompanied by abdominal discomfort. The loss of normal reflexes controlling defecation contributes significantly to these problems.
Loss of rectal sensation means patients cannot feel when the rectum is full or distinguish between gas and solid matter, leading to unexpected soiling.
Saddle Anaesthesia and Sensory Changes
The term "saddle anaesthesia" describes the characteristic pattern of numbness affecting areas that would contact a horse's saddle, including the perineum, inner thighs, buttocks, and genital regions.
Progressive numbness typically begins in the perianal area and spreads outward. Patients often describe this as a gradual loss of feeling, sometimes progressing from tingling sensations to complete numbness over several hours.
Altered genital sensation significantly impacts sexual function and intimate relationships. Both men and women report decreased or absent sensation during sexual activity.
Changes in temperature and pain sensation in the saddle region create dangerous situations where patients cannot feel injuries or pressure sores developing.
Motor Weakness and Mobility Issues
Lower limb weakness develops in approximately 60-80% of post-operative CES cases, ranging from subtle changes to significant impairment.
Foot drop represents one of the most noticeable motor deficits, affecting up to 30% of patients undergoing complex spinal procedures. This condition makes it impossible to lift the front part of the foot, causing a characteristic high-stepping gait.
Bilateral leg weakness distinguishes post-operative CES from more common single nerve root injuries. Patients struggle with activities requiring leg strength, such as:
- Climbing stairs
- Rising from chairs
- Walking extended distances
- Maintaining balance
Progressive muscle weakness can develop gradually over days, making early detection challenging.
The Underlying Mechanisms
Mechanical Compression
Post-operative mechanical compression occurs through various mechanisms:
Epidural haematomas develop in approximately 30% of cases, creating space-occupying lesions that compress nerve roots. These typically manifest within 24-48 hours of surgery.
Instrumentation malposition affects about 36% of cases. Misplaced screws, cages, or other hardware can directly compress neural structures.
Inadequate decompression contributes to roughly 17% of cases, where insufficient removal of compressive tissue leaves nerves vulnerable to post-operative swelling.
Vascular Insufficiency
The ischaemic theory of post-operative CES gains increasing recognition. The cauda equina receives blood supply from delicate vessels that can be disrupted during surgery or compromised by post-operative swelling.
Venous congestion occurs when post-operative oedema compresses the epidural venous plexus, creating dangerous increases in pressure around nerve roots.
Arterial insufficiency develops when surgical trauma compromises the already tenuous blood supply to nerve roots below the conus medullaris.
Timing and Progression Patterns
Acute Onset (0-48 Hours)
Rapid-onset symptoms developing within 48 hours typically indicate mechanical compression from haematoma or instrumentation problems. Epidural haematomas cause symptoms most quickly, with an average onset of 1.4 days post-operatively.
Delayed Onset (2-7 Days)
Nerve root oedema typically manifests later, with symptoms appearing an average of 4.8 days post-operatively. This delayed presentation can lead to misdiagnosis or delayed recognition.
Progressive vs. Stable Symptoms
Progressive worsening of symptoms over hours or days constitutes a surgical emergency requiring immediate intervention. The distinction between progressive and stable presentations guides critical treatment decisions.
Recovery and Long-Term Outlook
Factors Affecting Recovery
Recovery from post-operative CES varies tremendously between patients:
Severity at onset correlates strongly with outcomes. Patients presenting with incomplete symptoms generally achieve better recovery than those with complete retention and total numbness.
Age and comorbidities significantly impact recovery potential. Younger patients and those without diabetes or vascular disease demonstrate better neurological recovery patterns.
Rehabilitation and Management
Comprehensive rehabilitation plays a crucial role in maximising recovery potential through multidisciplinary teams including physiotherapists, occupational therapists, and continence specialists.
Bladder retraining programmes help patients regain continence through:
- Scheduled voiding protocols
- Pelvic floor exercises
- Gradual catheter weaning
- Continence aids when necessary
Mobility and strength training address motor deficits through targeted exercises, gait training, and assistive device provision.
Long-Term Outcomes
Studies reveal that whilst complete recovery occurs in a minority of cases, significant functional improvement is achievable for most patients with appropriate treatment.
Bladder function shows the most potential for recovery, with up to 67% of patients regaining meaningful control within 6-12 months. However, approximately 33% continue experiencing some degree of long-term dysfunction.
Bowel function recovery varies widely, with some patients achieving complete control whilst others require ongoing management strategies.
Sexual function often shows limited recovery, particularly regarding sensation. However, with appropriate counselling and medical interventions, many patients can achieve satisfying intimate relationships.
Prevention and Risk Reduction
Surgical Technique Considerations
Gentle tissue handling during surgery minimises trauma to neural structures. Experienced surgeons emphasise careful retraction, avoiding excessive manipulation of nerve roots, and maintaining adequate visualisation.
Appropriate decompression levels ensure adequate space for neural elements whilst avoiding unnecessary extensive surgery.
Meticulous haemostasis reduces the risk of post-operative haematoma formation, particularly attention to epidural vein bleeding control.
Post-Operative Monitoring
Regular neurological assessments during the immediate post-operative period enable early recognition of developing problems.
Patient education about symptoms to report empowers individuals to seek help immediately when concerning changes occur.
Early mobilisation protocols when medically appropriate allow for neurological monitoring during activity.
When to Seek Immediate Help
Patients and families must understand when to contact healthcare providers immediately:
- Any new or worsening bladder problems
- Progressive numbness in the saddle region
- Developing leg weakness
- Loss of bowel control
- Sexual dysfunction following normal post-operative recovery
Healthcare providers should maintain a high index of suspicion during post-operative care. The rarity of post-operative CES can lead to delayed recognition, but the consequences of missed diagnosis are severe.
Conclusion
Post-operative cauda equina syndrome represents a challenging complication that can transform a successful surgical outcome into a life-altering condition. Recognition of the varied symptom presentations, from bladder dysfunction and bowel problems to sensory changes and motor weakness, enables prompt intervention that may preserve neurological function.
The complex interplay of mechanical compression, vascular insufficiency, and inflammatory responses creates diverse clinical presentations requiring individualised assessment and management. Whilst complete recovery remains uncommon, significant functional improvement is achievable through prompt recognition, appropriate treatment, and comprehensive rehabilitation.
The key to optimal outcomes lies in education—of patients about symptoms to report, surgical teams about risk factors and prevention, and healthcare providers about recognition and management. Early recognition saves function, swift action preserves hope, and comprehensive care maximises potential for meaningful recovery.
References
- NCBI - Non-compressive postoperative cauda equina syndrome following decompression surgery - https://pmc.ncbi.nlm.nih.gov/articles/PMC6301535/
- PubMed - Cauda equina syndrome as a postoperative complication of lumbar spine surgery - https://pubmed.ncbi.nlm.nih.gov/15202877/
- PubMed - Cauda equina syndrome as a postoperative complication in five patients - https://pubmed.ncbi.nlm.nih.gov/11224866/
- World Journal of Clinical Cases - Cauda equina syndrome with urinary retention post-surgery - https://www.wjgnet.com/2307-8960/full/v13/i10/101796.htm
- Wikipedia - Cauda equina syndrome overview and symptoms - https://en.wikipedia.org/wiki/Cauda_equina_syndrome
- Surgical Neurology International - Post L5-S1 surgery cauda equina syndrome cases - https://surgicalneurologyint.com/surgicalint-articles/cauda-equina-syndrome-after-l5-s1-posterior-decompression-surgery-showing-a-convexity-sign-caused-by-engorgement-of-the-ventral-epidural-venous-plexus-a-case-series/
- NCBI - Cauda Equina Syndrome Following Decompression for Spinal Stenosis - https://pmc.ncbi.nlm.nih.gov/articles/PMC3864468/
- Cleveland Clinic - Cauda Equina Syndrome symptoms and treatment - https://my.clevelandclinic.org/health/diseases/22132-cauda-equina-syndrome
- NCBI - Neurogenic bladder in spinal cord injury patients - https://pmc.ncbi.nlm.nih.gov/articles/PMC4467746/
- NCBI - Long-term recovery outcomes assessment - https://pmc.ncbi.nlm.nih.gov/articles/PMC11254269/